According to the California Mental Health Services Authority, the following are goals set for integrated behavioral healthcare:
- Increase availability and quality of integrated health, mental health, substance use, and social services
- Promote access to care and reduce stigma
- Improve treatment outcomes and measures
- Strengthen care coordination between mental health and primary care providers
- Create collective impact through strong networks and collaborative partnerships
To become an integrated behavioral health clinician, a licensed professional must earn additional specialization through a certified integrated behavioral health continuing education program.
Integrated Behavioral Health Model
The National Council for Mental Wellbeing defines integrated services as the coordination and provision of a treatment team for physical and behavioral health conditions with attention to social determinants of health. Primary care targets physical health, while behavioral health encompasses mental health and substance use disorders. The integration of primary and behavioral healthcare relies on evidence-based research.
Integrated behavioral healthcare strives to create an inclusive communication network between all health providers for a given patient. This perspective also encourages healthcare providers to reflect beyond physical or mental ailments and consider environmental situations. Integrated health looks like psychological care with the understanding that simultaneously checking in with a primary care provider is more effective than treating patients for mental illness with psychological treatment alone.
Integrated Behavioral Health Solutions
In a report by the National Council for Mental Wellbeing funded by the Substance Abuse and Mental Health Services Administration, Designing, Implementing and Sustaining Physical Health-Behavioral Health Integration outlines eight key elements of integrated care to address physical health, behavioral health, and social determinants of health.
- Screening, Referral and Follow-up: This is the initial intake, assessment, and evaluation stage. The screening stage allows healthcare specialists to identify illnesses, create treatment plans, and track improvement measures.
- Prevention and Treatment of Common Conditions: The focus is on prevention, sometimes through medication. Examples of preventative healthcare include suicide risk screenings, physical health risk screenings, opioid screenings, and developmental screenings.
- Continuing Care Management: This encompasses longitudinal clinical monitoring and engagement. Continuing care management includes the referral network between physical and mental health providers.
- Self-Management Support: There are tools for patient activation and recovery regardless of literacy, financial status, and culture. Appointment reminders are an example of self-management support.
- Multidisciplinary Teamwork: An integrated care team who shares treatment info and care plans. Care teams generally begin with a primary care provider and then branch to external physical and psychological healthcare providers.
- Systematic Measurement and Quality Improvement: Quality metrics utilize screenings from the initial stage to improve healthcare. Quality improvement occurs by measuring current health states to previously reported baselines. This also contributes to improvements in disparities with measurable data.
- Linkage with Community/Social Services for Social Determinants of Health: This includes providing connections to housing and social support systems. Integrated healthcare specialists relay service organizations and resources. They may also act as case coordinators.
- Financial Sustainability: The process of billing and outcome reporting strives to limit attempts for billing with proper funding and transparent charges. Integrated healthcare does not refer to a centralized billing system between health disciplines, but rather the collaborative effort of multiple fields to ensure a patient’s unabridged care.
Four-Quadrant Clinical Integration Model
The Four-Quadrant Clinical Integration Model is a tool to assess patients depending on the risk and complexity of their physical and behavioral health. All quadrants include standard care by a primary care provider. Then, there are varying levels of psychological treatment depending on the patient’s needs.
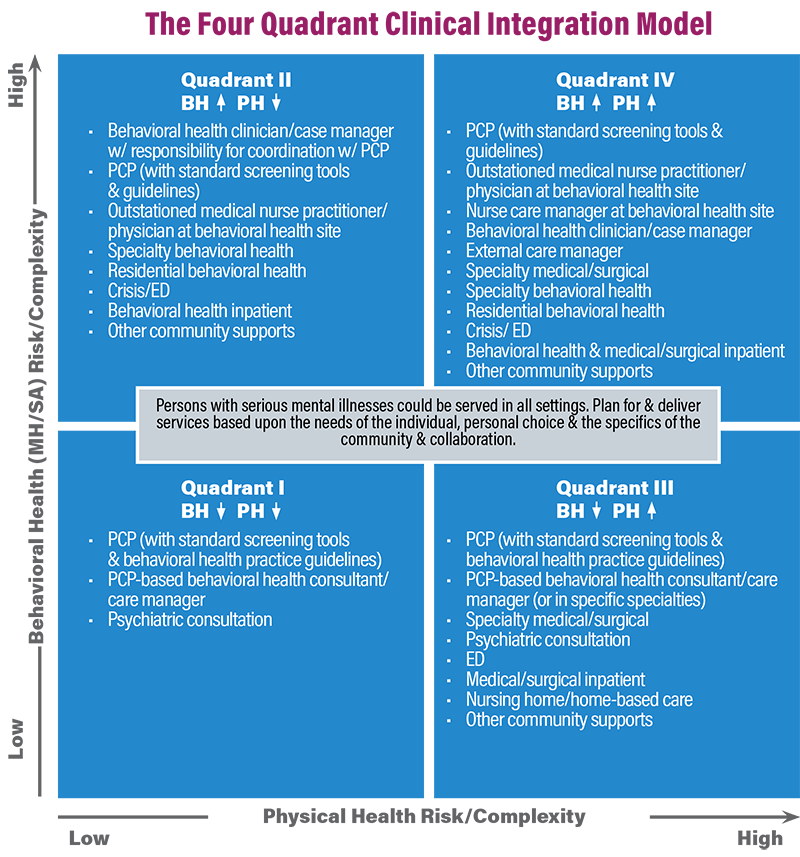
Each quadrant is listed below:
- Low Behavioral and High Physical Health Risk/Complexity
- PCP, Psychiatric Consultation
- Low Behavioral and Low Physical Health Risk/Complexity
- PCP, Psychiatric Consultation
- High Behavioral and High Physical Health Risk/Complexity
- PCP, Outstation medical nurse or physician, Specialty Behavioral Health and Physical Health
- High Behavioral and Low Physical Health Risk/Complexity
- PCP, Outstation medical nurse or physician, Specialty Behavioral Health
Regardless of physical health risk, mental health professionals administer a psychiatric consultation in the case of low behavioral risk and complexity. Lower-risk patients receive treatment from a primary care provider in addition to a psychological evaluation. Higher-risk patients require additional assessments, specialty care providers, and outstation care.
Integrative Healthcare Examples
Integrated behavioral healthcare grows with support as organizations and universities dedicate task forces toward uniting separate health disciplines. California, Colorado, and Washington are among the first states to incorporate federal funding for integrated behavioral healthcare, also referenced as integrated care or collaborative care.
Examples at the national level:
- California - The Integrated Behavioral Health Partners (IBHP) - The IBHP is a Californian organization focusing on expanding integrated healthcare practices across healthcare sectors. The IBHP has developed a mentoring program in addition to online accessible toolkits to promote integrated care.
- New York - New York State Collaborative Care Initiative - New York’s collaborative care initiative is a project funded by the New York Office of Mental Health in partnership with Washington University’s AIMS. Collaborative care intends to tackle illnesses like depression or anxiety more commonly in a primary care provider setting.
- Washington - Advancing Integrated Mental Health Solutions (AIMS) - AIMS funds and partners with national organizations to find solutions in various states, for example, the Texas Integrated Health Care Program and the Alaska Integrated Care for Depression and Substance Abuse. The Advancing Integrated Mental Health Solutions Center contributes to the foundation and structure of a plethora of programs nationally.
Examples at the community level:
- 988 - 988 is a new hotline solely responsible for mental health crises. This accessible 24/7 line redirects callers to local hotlines to access necessary resources for their situation. Frequently, callers utilize the resource for treatment by either a behavioral health clinician or primary care provider.
- Crisis Assessment Team - Crisis Assessment Teams consist of multidisciplinary teams of staff with the resources to provide psychiatric and physical evaluations. Each county directs funding to its location-specific team. For example, San Francisco Mobile Crisis has a separate unit from its neighboring Alameda County Mobile Crisis Team.
Examples at the individual level:
- Pain Management for Veterans
- Symptom Management in Cancer Patients - According to the National Center for Complementary and Integrative Health (NCCIH), integrative care improves situations for veterans and cancer patients requiring pain or symptom management. When managing treatment for veterans or cancer survivors, their physical health is taken into account by their primary care provider in addition to their psychological health with an in-network mental health provider.
Integrated Behavioral Health Training
Integrated behavioral health clinicians begin with the same foundational mental health background as traditional therapists and counselors. With a master’s or Ph.D. degree, a clinician needs to advance their education depending on which areas they feel are the best fit for their practice. Mental healthcare specialists need to complete an integrated behavioral health training program. Certain programs directly emphasize the multi-field approach.
Collaborative care networks require clinicians who cooperate with and understand fields outside of their own. To decide which areas of integrated behavioral healthcare are of interest, examine local networks of accessible healthcare specialists and explore continuing education credits in those subjects.
To ensure readiness as an integrated behavioral health clinician, follow this collaborative care readiness checklist from the University of Washington Psychiatry and Behavioral Services, which summarizes readiness milestones for care providers.
- Do you have the involvement or support of senior or clinic leadership?
- Are primary care providers and other physical health providers integrated? Who are the primary care provider planner and trainers?
- What are staffing plans for behavioral healthcare managers? Will services be in-person or through telehealth?
- Who is the psychiatric care provider, and how will you access their services when needed?
- How will you track patient outcomes and progress?
- How will you ensure the longevity of staffing resources and finances?
- Do program leads, and behavioral health supervisors have what they need to implement change?
- What are evidence-based methodologies utilized in practice outside of medicine?
- What does the behavioral health screening look like, and how is staff trained on the screening?
- What is your plan for patients who are at risk of suicide?
Integrated Behavioral Health Specializations
Below are a few specialties in integrated behavioral health care:
- Suicide Prevention Training
- Primary Care Provider Training
- Psychiatric Consultant Training
- Behavioral Health Care Manager Training
Integrated Behavioral Health Certificate Program
Dr. Jerrod Brown, Ph.D., is an integrated behavioral healthcare specialist who holds not only psychological credentials but also nutrition, stress, and sleep certifications. Consider the following courses led by Dr. Brown, founder and CEO of the American Institute for the Advancement of Forensic Studies, as an introduction to integrated behavioral health as a clinician.
- Integrated Behavioral Health: An Overview with Dr. Jerrod Brown, Ph.D.
- Trauma-Informed Integrated Behavioral Healthcare with Dr. Jerrod Brown, Ph.D.
- Integrated Behavioral Health Subscription with Jerrod Brown, Ph.D., as he presents a live 10-program series
CONCEPT Continuing and Professional Studies will soon release an Integrated Behavioral Health Certificate Program for licensed professionals with an interest in specializing their skills and providing collaborative care, available in 2023.
Integrated Behavioral Health Jobs
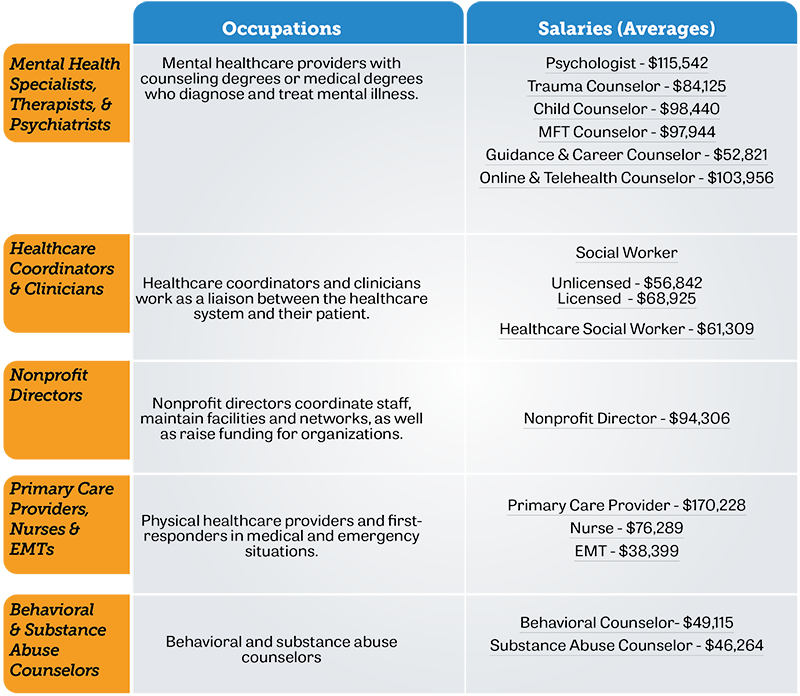
Integrative mental health jobs pay an average of $96,450 with an ability to earn up to $142,500, according to ZipRecruiter.
The following list shows average salaries for various occupations* that are part of the network of care providers used in integrated behavioral health, including mental health providers, PCPs, nonprofit directors, and more:
Note: The salaries listed below are for each occupation in general, rather than solely representing those that specialize in integrated behavioral health. Actual salaries may reflect higher values given the level of specialization and additional education.
Social Work and Integrated Healthcare
Social workers occupy distinctive spaces in healthcare as they provide case management in addition to therapeutic treatment plans because of their various expertise. A social worker utilizes integrated care by connecting their client to resources, such as access to physical healthcare providers, groceries, housing, or welfare. To be an integrated behavioral health social worker, additional training includes fields of specialization. Social workers are most likely to work in an integrated healthcare setting as they are a point of contact between providers and resources to their clients.
Examples of specialization include healthcare coordination, working with children or the elderly, or online telehealth counseling. Social workers deal with several of the following demographics: elderly, children, disabled, schools, healthcare, substance abuse, and more.
Integrated Healthcare for Psychology and Counseling
Psychologists and counselors work with physical healthcare providers, such as psychiatrists and general practitioners, to promote their client’s recovery. Psychologists and counselors in integrated behavioral health require a solid communication network between multidisciplinary staff with various educational backgrounds. Mental health specialists build rapport with coworkers in various fields of study. A therapist or counselor needs a secure referral system for when a client needs medication from a psychiatrist or primary care provider, which is outside of their traditional scope of practice as a mental healthcare specialist.
The American Psychological Association provides an introductory set of videos demonstrating how psychologists in integrated healthcare are practical in pediatric primary care, OB/GYN, family medicine, and geriatrics.























