Mental Health and Suicidal Crises
A mental health crisis looks different depending on the individual. Some cases that qualify as a crisis include substance abuse or addiction, untreated mood or psychotic disorder, and lack of housing.
Callers who do not feel suicidal are able to use the crisis hotline services as well. However, if there are many high-risk or distressed callers, they will need to call back at a different time. Callers may lack a proper support system, and 988 offers a solution. These preventative care steps and subsequent follow-up programs support the mental health of communities.
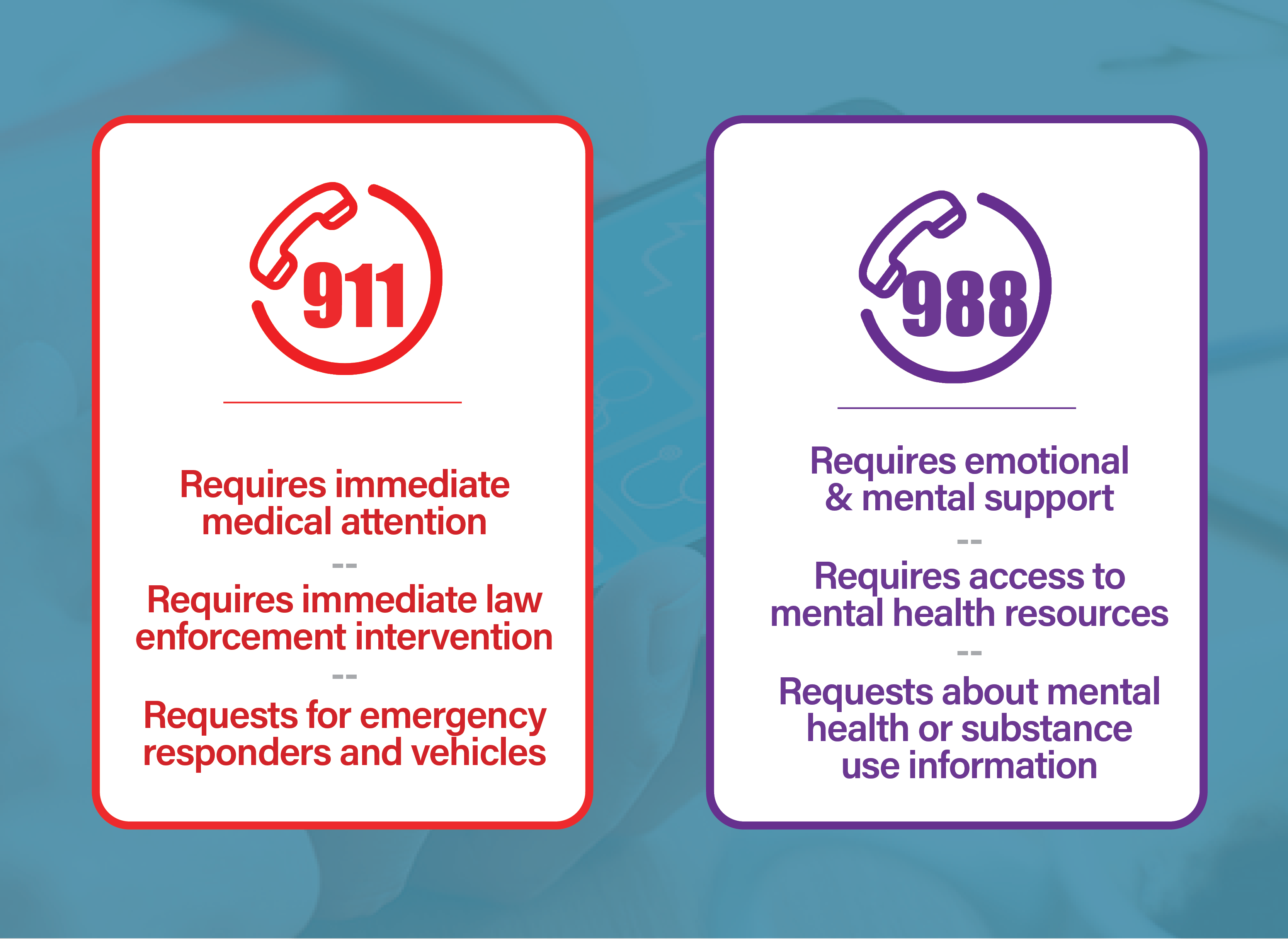
Sometimes, individuals share suicidal thoughts, but they either don’t have a plan or the means to act on these thoughts. This would not be a reason to call an emergency number like 911. Many times, suicidal individuals just want to discuss their feelings without the threat of forced hospitalization or police interference.
988 is the ideal way to connect suicidal individuals with a trained counselor. The American Association of Suicidology accredits crisis centers. The organization certifies volunteers, interns, and supervisors meet exemplary standards when providing care to the community.
To connect patients to the proper resources, the crisis lines redirect callers to their local county hotline. Make sure to pass along a location-specific number to ensure a seamless transition for a client moving counties or states.
Mobile Crisis Units
Mobile crisis teams can be requested through 988. A mobile crisis unit is a team composed of a mental health provider and a public safety official. The pair is able to travel to individuals in their communities.
The team is able to complete crisis interventions such as welfare checks, evaluation for hospitalizations, and consultations to other behavioral health or public safety officials. Varying by community, the public safety official may be a law enforcement official or they may be a paramedic.
There are distinctions between each county’s mobile crisis team, but all generally provide accessible mental healthcare.
- Berkeley’s MCT is the Mobile Crisis Team. Berkeley is located in Alameda County and is home to three different mobile crisis models. There’s a team with a police officer and licensed clinician, a licensed clinician and an EMT, and a duo of licensed clinicians.
- Denver’s STAR is short for Support Team Assisted Response. Denver in Colorado is unique because they partner their behavioral health official with a paramedic. The team attends to calls in their streetwear.
- South Florida’s MRT is the Mobile Response Team. The Apalachee Center of South Florida, in particular, provides an opportunity to receive telehealth services after hours in partnership with County Sherrif’s Department.
Mobile crisis units are not able to come to the scene to assess an individual if there is a weapon present, violent behavior, or in a high-risk area (such as a bridge). Dr. Stephen D. Hart, Ph.D., discusses mental disorder and violence risk in a program explaining the direct and indirect links between the two.
Request a Crisis Intervention Team
How law enforcement perceives individuals in the public affects the type of healthcare treatment they receive. When an officer is trained in crisis intervention or paired with a social worker who is, these police and public safety officials are more likely to deescalate a crisis. Untreated mental illness looks threatening to those who do not have the experience to treat it as a healthcare issue.
The first Crisis Intervention Team came as a response to the death of Joseph Dewayne Robinson after a mishandled mental health crisis in Memphis, Tennessee.
Because of accessibility issues, mental healthcare falls short and individuals who require treatment often find themselves imprisoned or hospitalized. According to the Journal of the American Academy of Psychiatry and the Law, approximately 1,000 individuals were fatally shot by police officers in 2018 and 25% of those shot were persons with mental illness. 988 is a service working to educate communities on public safety and provide access to 24/7 mental healthcare.
Public Safety Officers and their Mental Health
Law enforcement officers who respond to mental health and suicidal crises interact with high-risk and violent situations often in their careers. A mental health crisis call holds the possibility of turning into a critical incident. There are professional public safety psychologists to help officers process these traumatic events. Examples of critical incidents include officer-involved shootings, child injuries, or death.
Dr. Nancy Bohl-Penrod and Dr. Jamie Brower, in partnership with the American Board of Police and Public Safety Psychology, provide an educational course for emergency responders and their families as a Critical Incident Response.