CBT vs DBT for Treating Specific Illnesses
Differential Effectiveness: CBT has demonstrated effectiveness in treating depression, anxiety, post-traumatic stress disorder, obsessive-compulsive disorder, phobias, panic disorder, and sleep issues. On the other hand, DBT, while originating from borderline personality disorder, has proven beneficial for eating disorders, substance-use disorders, trauma survivors, and conditions involving self-harm.
Philosophical Foundations: CBT is inspired by stoic philosophy and the Socratic Method, which emphasize logic and reason. On the other hand, DBT is rooted in mindfulness skills derived from Buddhism and Zen practices, which promote acceptance of pain and the impermanence of the world. These philosophical foundations are integrated into the CBT and DBT frameworks, reflecting a diverse approach to mental health that combines both Western and Eastern perspectives in addressing cognitive and emotional challenges. Individuals can blend ancient wisdom and modern psychological principles by engaging in these therapeutic modalities to develop a holistic understanding of themselves and promote sustainable well-being.
Understanding Cognitive Behavioral Therapy (CBT)
CBT, a cornerstone of evidence-based psychotherapy, serves as a versatile tool for addressing a spectrum of mental health challenges, including depression, anxiety, PTSD, and substance-use disorders.
How CBT Works
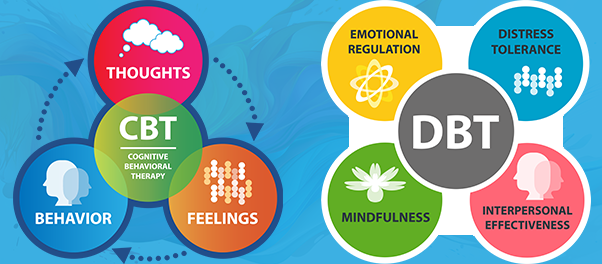
At its core, CBT operates on the premise that thoughts shape beliefs, beliefs influence behavior, and this chain of effects extends to emotions. Techniques employed in CBT include reevaluating negative thoughts, relaxation, confronting fears, developing coping skills, and enhancing self-confidence and self-esteem.
Delivery
Structured as a short-term intervention, CBT is goal-oriented and present-focused. Its adaptability allows for application in various settings, both face-to-face and virtually.
Structure and Focus
CBT is structured, short-term, goal-oriented, and concentrates on the present. Generally, sessions may commence with education on the specific mental health issue, followed by skill-building exercises such as problem-solving and realistic thinking. These skills empower individuals to create positive changes in their thoughts, emotions, and behaviors, enabling effective problem-solving in the future.
Integration with Psychotherapy
CBT, classified as a form of psychotherapy or "talk therapy," involves collaboration with a mental health professional. Through this partnership, individuals gain insights into their challenges and acquire skills to manage them independently.
Learning from CBT
In CBT, individuals learn about the intricate connections between thoughts, feelings, and behaviors. For instance, negative beliefs may lead to avoidance behaviors, resulting in feelings of loneliness. Positive changes in any of these factors can catalyze positive transformations. Research supports CBT's effectiveness in addressing diverse mental health problems, including depression, anxiety disorders, eating disorders, and substance use problems.
CBT Philosophy
CBT is rooted in examining how thoughts, feelings, and behaviors influence each other. It empowers individuals to use logic and reason to take control of their thoughts. This approach, often drawing from stoic philosophy and the Socratic Method, is particularly effective for conditions like depression and anxiety.
Delving into Dialectical Behavior Therapy (DBT)
DBT is an evolution of CBT with an enhanced focus on emotional and social aspects, originated as a means to help individuals cope with extreme emotions and harmful behaviors. Initially designed for borderline personality disorder, DBT has shown efficacy in addressing various mental health concerns, especially those involving self-harm.
How DBT Works
DBT builds upon CBT principles but emphasizes emotional and social dimensions more. It strives to assist individuals in managing intense emotions and curbing harmful behaviors. DBT is recognized as an evidence-based approach. It's applied to diverse mental health challenges, including mood and anxiety disorders, eating disorders, substance use disorders, PTSD, ADHD, self-harm, chronic pain, and stress management. DBT's adaptability lies in its focus on skill-building, mindfulness, and behavioral techniques, making it effective for a broad range of emotional and behavioral difficulties.
Integration with Psychotherapy
Similar to CBT, DBT involves collaboration with a mental health professional. The therapist-client relationship is crucial; regular check-ins provide opportunities to discuss successes and challenges. Treatment incorporates a blend of one-on-one sessions and group sessions.
Learning from DBT
DBT introduces key differences from CBT, emphasizing the validation of experiences and the cultivation of self-acceptance despite challenges. The importance of relationships, including the therapeutic alliance, is underscored. In addition to CBT skills, individuals in DBT learn techniques for emotion regulation, building relationships, coping with distress, fostering acceptance, and practicing mindfulness.
Integrating New Information
Recognizing the unique characteristics of DBT, it focuses on helping individuals acknowledge pain, feel safe in the moment, and choose healthy behaviors. It extends beyond thoughts to identify triggers and match them with healthy coping mechanisms.
Tailoring Treatment Choices to Your Needs
Considerations: The decision between CBT and DBT hinges on individual needs and goals. While both are evidence-based and practical, nuances in treatment duration and the approach to handling negative emotions influence the choice.
Specific factors influencing the selection include:
Duration of Treatment:
- CBT often follows a relatively structured and time-limited format. It is typically designed for short- to medium-term interventions, with treatment durations ranging from a few weeks to several months. It is well-suited for individuals looking for a focused approach to address specific issues within a defined timeframe.
- DBT is often implemented in longer-term treatment plans. It includes individual therapy and skills training groups, with the comprehensive program lasting around six months to a year. DBT is suitable for individuals requiring ongoing support for emotional regulation and interpersonal challenges.
Handling Negative Emotions:
- CBT focuses on identifying and challenging negative thought patterns and beliefs. It helps individuals develop more adaptive thinking patterns and behaviors. The emphasis is on changing cognitive processes to influence emotions and behaviors.
- DBT places a significant emphasis on accepting and validating emotions while simultaneously working on changing problematic behaviors. It includes specific skills training modules for emotion regulation, distress tolerance, and interpersonal effectiveness.
Targeted Issues:
- CBT is versatile and can be applied to a wide range of mental health issues, including anxiety, depression, and various mood disorders. It is goal-oriented and problem-focused, making it practical for addressing specific symptoms.
- As previously mentioned, DBT was initially developed for individuals with borderline personality disorder and has since been adapted for various conditions. It is particularly effective for individuals struggling with emotional dysregulation, self-harm, and interpersonal difficulties.
Individual Preferences and Readiness for Change:
- Individual preferences and readiness for change play a crucial role in the decision. Some individuals may prefer the structured nature of CBT, while others may resonate with the acceptance-based approach of DBT.
- Individuals prepared for a focused and relatively short-term intervention may lean towards CBT. In contrast, those who recognize the need for ongoing support and skill-building, particularly in managing complex emotional experiences, may find DBT more aligned with their readiness for sustained change.
Therapeutic Relationship:
- Understanding individual preferences involves considering the therapeutic style that resonates with the person seeking treatment. Some individuals may feel more engaged and motivated in a structured and directive therapeutic setting, appreciating the step-by-step guidance offered by CBT. Others may connect more with the dialectical and collaborative nature of DBT, valuing the emphasis on acceptance and change as integral components of the therapeutic process.
Effectiveness:
- CBT demonstrates efficacy across a range of mental health conditions, while DBT shines in addressing specific challenges, including BPD, self-harm tendencies, and suicidal ideation.
Harmonizing DBT and CBT: A Holistic Approach
Background: Given DBT's roots in CBT, there's potential for integration. Both therapies share the common goal of modifying maladaptive behaviors to alleviate emotional distress.
Considerations: While CBT boasts a more extended history of established effectiveness, DBT is still under study for its broad applicability. Integrating both approaches offers a comprehensive strategy that leverages the strengths of each.
.
Additional Resources
Blog Post
- What is Evidence-Based Therapy?
- Pros and Cons of DBT Therapy
- Trauma-Focused Cognitive Behavioral Therapy
- Cognitive Behavioral Therapy for Insomnia
- Cognitive Behavioral Therapy for Anxiety
- Personality Disorders
Research
Podcast
Deepen your DBT Knowledge with a Free Intro to DBT eBook or Free Advanced DBT eBook to Maintain a Competitive Edge.