Prevalence
The national lifetime prevalence estimate for PTSD using DSM-IV criteria is approximately 6.8% for U.S. adults and 5.0% to 8.1% for adolescents. Currently, comprehensive population-based data using DSM-5 are unavailable; however, findings are beginning to emerge. For example, in two U.S. epidemiological studies, lifetime DSM-5 PTSD prevalence estimates ranged from 6.1% to 8.3%.
Rates of PTSD are higher among veterans and others whose vocation increases the risk of traumatic exposure (e.g., police, firefighters, and emergency medical personnel). In addition, the highest rates of PTSD are found among survivors of rape, military combat and captivity, and ethnically or politically motivated internment and genocide.
Racial differences show higher rates of PTSD among U.S. Latinx, African Americans, and American Indians compared with Whites. Potential reasons for these variations include differences in predisposing factors, such as exposure to past adversity, racism, and discrimination, and availability or quality of treatment, social support, socioeconomic status, and other social resources that facilitate recovery and are confounded with race and ethnicity.
Development and Course
After the first year of life, PTSD can occur at any age. Symptoms usually start within the first three months after the trauma, although there may be a delay of months or even years before the full criteria for the diagnosis are met.
Duration of PTSD symptoms also varies, with complete recovery within three months occurring in approximately one-half of adults. However, some individuals remain symptomatic for over 12 months and sometimes more than 50 years. In addition, symptom recurrence and intensification may occur in response to reminders of the original trauma, ongoing life stressors, or newly experienced traumatic events.
Children aged six and younger may develop PTSD due to severe emotional abuse (e.g., the threat of abandonment), which can be perceived as life-threatening. In addition, treatment for life-threatening illnesses (e.g., cancer, organ transplantation) may contribute to the risk of developing posttraumatic stress symptoms.
Young children are likelier to express reexperiencing symptoms through play that refers directly or symbolically to the trauma. In addition, parents may report emotional or behavioral changes in young children. Because of young children’s limitations in expressing thoughts or labeling emotions, negative mood or cognition alterations tend to involve mood changes primarily. In addition, children may experience co-occurring traumas (e.g., physical abuse, witnessing domestic violence) and, in chronic circumstances, may be unable to identify the onset of symptomatology.
Irritable or aggressive behavior in children and adolescents can interfere with peer relationships and school behavior. Reckless behavior may lead to accidental injury to self or others, thrill-seeking, or high-risk behaviors. In older individuals, the disorder is associated with adverse health perceptions, primary care utilization, and suicidal thoughts. In addition, declining health, worsening cognitive functioning, and social isolation may exacerbate PTSD symptoms.
Risk and Prognostic Factors
The cause of PTSD is unknown, but psychological, genetic, physical, and social factors are involved. PTSD changes the body’s response to stress and affects an individual’s stress hormones and neurotransmitters. Individuals exposed to trauma in the past may be at an increased risk for developing PTSD. Risk factors for PTSD can operate in many ways, including predisposing individuals to trauma or extreme emotional responses when exposed to traumatic events.
Pretraumatic Factors
Risk Factors
- Lower socioeconomic status
- Lower education
- Exposure to prior trauma (especially during childhood)
- Childhood adversity (e.g., economic deprivation, family dysfunction, parental separation, or death)
- Lower intelligence
- Ethnic discrimination and racism
- Family psychiatric history
Protective Factors
- Social support, before event exposure, is an important protective factor against PTSD
Peritraumatic Factors
- The severity of the trauma
- Perceived life threat
- Personal injury
- Dissociation, fear, and panic during the trauma and persists afterward
- Interpersonal violence: trauma perpetrated by a caregiver or a witnessed threat to a caregiver
- Military personnel: being a perpetrator, witnessing atrocities, or killing the enemy
Posttraumatic Factors
Risk Factors
- Negative appraisals
- Inappropriate coping strategies
- Development of acute stress disorder
- Exposure to repeated upsetting reminders
- Subsequent adverse life events
- Financial or other trauma-related losses
- Forced migration and high levels of daily stressors
- Exposure to racial and ethnic discrimination
Protective Factors
- Social support (e.g., family stability for children) is a protective factor that moderates outcomes after trauma
Culture-Related Diagnostic Issues
Different demographic, cultural, and occupational groups have different levels of exposure to traumatic events, and the relative risk of developing PTSD following a similar level of exposure (e.g., religious persecution) may also vary across cultural, ethnic, and racialized groups.
In many populations worldwide, there are cultural concepts of distress resembling PTSD and are characterized by diverse manifestations of psychological distress attributed to frightening or traumatic experiences. Thus, cultural ideas of distress influence the expression of PTSD and the range of its comorbid disorders.
Factors that Influence the Risk of Onset & Severity of PTSD
- The type of traumatic exposure (e.g., genocide)
- The impact on disorder severity of the meaning attributed to the traumatic event (e.g., inability to perform funerary rites after a mass killing)
- The ongoing sociocultural context (e.g., residing among unpunished perpetrators in postconflict settings)
- Exposure to racial and ethnic discrimination
- Other cultural factors (e.g., acculturative stress in migrants)
Cultural Concepts of Distress
Some communities are exposed to pervasive and ongoing traumatic environments rather than isolated events; in these communities, the predictive power of individual traumatic events for developing PTSD may diminish. In cultures where social image (e.g., maintaining a family’s “face”) is emphasized, public defamation or shaming may magnify the impact of events. Lastly, some cultures may attribute PTSD syndromes to negative supernatural experiences.
The Clinical Expression of Symptoms
In many non-Western groups, avoidance is less commonly observed, whereas physical symptoms (e.g., dizziness, shortness of breath, heat sensations) are more common. Other symptoms that vary are distressing dreams, amnesia unrelated to head injury, and reckless but non-suicidal behavior. Negative moods, especially anger, are common cross-culturally in individuals with PTSD, as are distressing dreams and sleep paralysis. In specific cultural contexts, it may be normative to respond to traumatic events with negative beliefs about oneself or spiritual attributions that may appear exaggerated to others. For example, blaming oneself may be consistent with ideas of karma in South and East Asia, destiny or “spoiled medicine law” in West Africa, and cultural differences in locus of control and conceptions of self.
Sex- and Gender-Related Diagnostic Issues
- PTSD is more prevalent among women than among men across the lifespan
- The lifetime prevalence of PTSD ranges from 8.0% to 11.0% for women and 4.1% to 5.4% for men
- Women in the general population experience PTSD for a longer duration than do men
- Research suggests that gender plays a role in PTSD diagnosis and the course of the illness within samples of justice-involved individuals
Increased Risk for Women
- Greater likelihood of exposure to childhood sexual abuse
- Sexual assault
- Other forms of interpersonal violence
- Gender differences in the emotional and cognitive processing of trauma
- Effects of reproductive hormones
Association With Suicidal Thoughts or Behavior
Traumatic events such as childhood abuse or sexual trauma increase an individual’s suicide risk in civilians (adults and adolescents) and veterans.
PTSD is associated with suicidal thoughts, suicide attempts, and death from suicide. In addition, the presence of PTSD has been associated with an increased likelihood of transitioning from suicidal thoughts to a suicide plan or attempt.
Functional Consequences of Posttraumatic Stress Disorder
PTSD is associated with high impairment in social, occupational, and physical functioning; reduced quality of life; and physical health problems. Impaired functioning is exhibited across social, interpersonal, developmental, educational, physical health, and occupational domains. PTSD is associated with poor social and family relationships, absenteeism from work, lower income, and lower educational and occupational success.
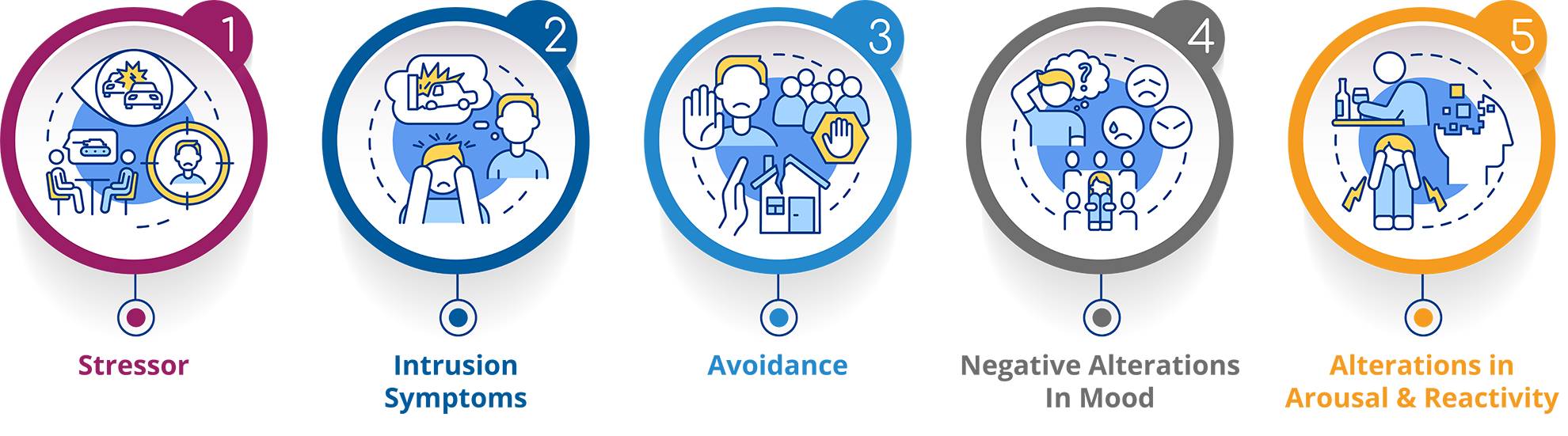
Symptoms
The symptoms of PTSD fall into four main categories:
Intrusion - "Reliving" the Event
- Recurrent, uncontrollable, and distressing memories
- Recurrent and upsetting trauma-linked dreams
- Dissociative reactions, including flashbacks where the event seems to be happening over and over
Avoidance
- Avoidance of trauma-related thoughts or feelings (internal stimuli)
- Avoid external trauma reminders (e.g., people, places, objects, situations, etc.)
Negative Alterations in Cognitions and Mood
Cognitions
- Inability to remember key features of the event
- Negative beliefs and expectations about oneself and the world
- Self-blame for trauma and its consequences
Emotions
- Negative trauma-related emotions (e.g., fear, shame)
- Diminished interest in activities
- Feeling alienated from others
- Inability to experience positive feelings
Alterations in Arousal and Reactivity
- Irritability or aggression
- Self-destructive or reckless behavior
- Hypervigilance
- Exaggerated startle response
- Difficulty concentrating
- Sleep disturbances
Additional Resources
Consider these resources for further insight into Post-Traumatic Stress Disorder.
Blog Posts
Training
- Assessing Allegations of Trauma in Forensic Contexts
- Psychological Evaluation in Personal Injury and Civil Rights Cases
Research






















